“The last of human freedoms – the ability to chose one’s attitude in a given set of circumstances.”
Why ‘Quality Care’ is dangerous
Interesting piece from The Wall Street Journal
Why ‘Quality’ Care Is Dangerous
The growing number of rigid protocols meant to guide doctors have perverse consequences.
By JEROME GROOPMAN and PAMELA HARTZBAND
The Obama administration is working with Congress to mandate that all Medicare payments be tied to “quality metrics.” But an analysis of this drive for better health care reveals a fundamental flaw in how quality is defined and metrics applied. In too many cases, the quality measures have been hastily adopted, only to be proven wrong and even potentially dangerous to patients.
Health-policy planners define quality as clinical practice that conforms to consensus guidelines written by experts. The guidelines present specific metrics for physicians to meet, thus “quality metrics.” Since 2003, the federal government has piloted Medicare projects at more than 260 hospitals to reward physicians and institutions that meet quality metrics. The program is called “pay-for-performance.” Many private insurers are following suit with similar incentive programs.
In Massachusetts, there are not only carrots but also sticks; physicians who fail to comply with quality guidelines from certain state-based insurers are publicly discredited and their patients required to pay up to three times as much out of pocket to see them. Unfortunately, many states are considering the Massachusetts model for their local insurance.
How did we get here? Initially, the quality improvement initiatives focused on patient safety and public-health measures. The hospital was seen as a large factory where systems needed to be standardized to prevent avoidable errors. A shocking degree of sloppiness existed with respect to hand washing, for example, and this largely has been remedied with implementation of standardized protocols. Similarly, the risk of infection when inserting an intravenous catheter has fallen sharply since doctors and nurses now abide by guidelines. Buoyed by these successes, governmental and private insurance regulators now have overreached. They’ve turned clinical guidelines for complex diseases into iron-clad rules, to deleterious effect.
One key quality measure in the ICU became the level of blood sugar in critically ill patients. Expert panels reviewed data on whether ICU patients should have insulin therapy adjusted to tightly control their blood sugar, keeping it within the normal range, or whether a more flexible approach, allowing some elevation of sugar, was permissible. Expert consensus endorsed tight control, and this approach was embedded in guidelines from the American Diabetes Association. The Joint Commission on Accreditation of Healthcare Organizations, which generates report cards on hospitals, and governmental and private insurers that pay for care, adopted as a suggested quality metric this tight control of blood sugar.
A colleague who works in an ICU in a medical center in our state told us how his care of the critically ill is closely monitored. If his patients have blood sugars that rise above the metric, he must attend what he calls “re-education sessions” where he is pointedly lectured on the need to adhere to the rule. If he does not strictly comply, his hospital will be downgraded on its quality rating and risks financial loss. His status on the faculty is also at risk should he be seen as delivering low-quality care.
But this coercive approach was turned on its head last month when the New England Journal of Medicine published a randomized study, by the Australian and New Zealand Intensive Care Society Clinical Trials Group and the Canadian Critical Care Trials Group, of more than 6,000 critically ill patients in the ICU. Half of the patients received insulin to tightly maintain their sugar in the normal range, and the other half were on a more flexible protocol, allowing higher sugar levels. More patients died in the tightly regulated group than those cared for with the flexible protocol.
Similarly, maintaining normal blood sugar in ambulatory diabetics with vascular problems has been a key quality metric in assessing physician performance. Yet largely due to two extensive studies published in the June 2008 issue of the New England Journal of Medicine, this is now in serious doubt. Indeed, in one study of more than 10,000 ambulatory diabetics with cardiovascular diseases conducted by a group of Canadian and American researchers (the “ACCORD” study) so many diabetics died in the group where sugar was tightly regulated that the researchers discontinued the trial 17 months before its scheduled end.
And just last month, another clinical trial contradicted the expert consensus guidelines that patients with kidney failure on dialysis should be given statin drugs to prevent heart attack and stroke.
These and other recent examples show why rigid and punitive rules to broadly standardize care for all patients often break down. Human beings are not uniform in their biology. A disease with many effects on multiple organs, like diabetes, acts differently in different people. Medicine is an imperfect science, and its study is also imperfect. Information evolves and changes. Rather than rigidity, flexibility is appropriate in applying evidence from clinical trials. To that end, a good doctor exercises sound clinical judgment by consulting expert guidelines and assessing ongoing research, but then decides what is quality care for the individual patient. And what is best sometimes deviates from the norms.
Yet too often quality metrics coerce doctors into rigid and ill-advised procedures. Orwell could have written about how the word “quality” became zealously defined by regulators, and then redefined with each change in consensus guidelines. And Kafka could detail the recent experience of a pediatrician featured in Vital Signs, the member publication of the Massachusetts Medical Society. Out of the blue, according to the article, Dr. Ann T. Nutt received a letter in February from the Massachusetts Group Insurance Commission on Clinical Performance Improvement informing her that she was no longer ranked as Tier 1 but had fallen to Tier 3. (Massachusetts and some private insurers use a three-tier ranking system to incentivize high-quality care.) She contacted the regulators and insisted that she be given details to explain her fall in rating.
After much effort, she discovered that in 127 opportunities to comply with quality metrics, she had met the standards 115 times. But the regulators refused to provide the names of patients who allegedly had received low quality care, so she had no way to assess their judgment for herself. The pediatrician fought back and ultimately learned which guidelines she had failed to follow. Despite her cogent rebuttal, the regulator denied the appeal and the doctor is still ranked as Tier 3. She continues to battle the state.
Doubts about the relevance of quality metrics to clinical reality are even emerging from the federal pilot programs launched in 2003. An analysis of Medicare pay-for-performance for hip and knee replacement by orthopedic surgeons at 260 hospitals in 38 states published in the most recent March/April issue of Health Affairs showed that conforming to or deviating from expert quality metrics had no relationship to the actual complications or clinical outcomes of the patients. Similarly, a study led by UCLA researchers of over 5,000 patients at 91 hospitals published in 2007 in the Journal of the American Medical Association found that the application of most federal quality process measures did not change mortality from heart failure.
State pay-for-performance programs also provide disturbing data on the unintended consequences of coercive regulation. Another report in the most recent Health Affairs evaluating some 35,000 physicians caring for 6.2 million patients in California revealed that doctors dropped noncompliant patients, or refused to treat people with complicated illnesses involving many organs, since their outcomes would make their statistics look bad. And research by the Brigham and Women’s Hospital published last month in the Journal of the American College of Cardiology indicates that report cards may be pushing Massachusetts cardiologists to deny lifesaving procedures on very sick heart patients out of fear of receiving a low grade if the outcome is poor.
Dr. David Sackett, a pioneer of “evidence-based medicine,” where results from clinical trials rather than anecdotes are used to guide physician practice, famously said, “Half of what you’ll learn in medical school will be shown to be either dead wrong or out of date within five years of your graduation; the trouble is that nobody can tell you which half — so the most important thing to learn is how to learn on your own.” Science depends upon such a sentiment, and honors the doubter and iconoclast who overturns false paradigms.
Before a surgeon begins an operation, he must stop and call a “time-out” to verify that he has all the correct information and instruments to safely proceed. We need a national time-out in the rush to mandate what policy makers term quality care to prevent doing more harm than good.
Dr. Groopman, a staff writer for the New Yorker, and Dr. Hartzband are on the staff of Beth Israel Deaconess Medical Center in Boston and on the faculty of Harvard Medical School.
The Monday Morning Quote #53
Slipped to Tuesday but that’s what West Cork does to me.
“Aim to enjoy your work instead of going the long way around!
Sacrificing happiness at work, to earn money, to buy back happiness in your personal life … is a very inefficient process!”
Paddi Lund
Don’t miss Paddi on his visit to the UK &Ireland in October. Have a look here.
How to Regain Your Life Balance in 15 Minutes
Here’s a blog posting from my client and friend Joanna Taylor on the value of self-hypnosis. Do take her up on her offer of the free CD it’ll do you no end of good.
The technique of self-hypnosis can help you to regain your life balance, using as little as 15 minutes a day.
Hypnosis allows the use of a deeply relaxing state in order that change can take place at the unconscious level; the power of hypnosis lies in the connection that is built with the unconscious mind.
Being able to use self-hypnosis can provide unmeasurable benefits, both physically and emotionally, and can help in achieving goals that otherwise might appear too difficult, or even impossible. Self-hypnosis is a way to connect with your own potentiality, your own infinite possibilities and your own creativity.
Clinical Hypnotherapist Joanna Taylor is running introductory courses in self-hypnosis at her Consultancy Offices in Pickering, North Yorkshire. See the website at www.joanna-taylor.co.uk for more details, and you can also request a free relaxation CD.
Resources – Fresh Business Thinking
Fresh Business Thinking is a useful website full of links to all sorts of information for the small business. They produce newsletters on a regular basis that are usually an interesting read.
Here’s the link www.freshbusinessthinking.com and here’s a recent article on making the most of your existing customers.
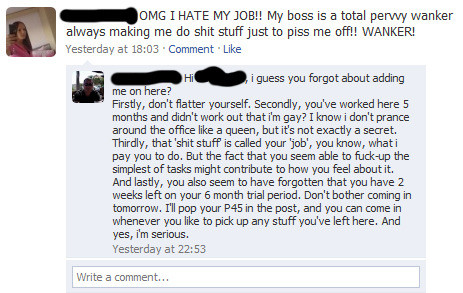
How To Lose Your Job On Facebook
The Monday Morning Quote #52
If you could actually stand in someone else’s shoes, to hear what they hear, see what they see, and feel what they feel,
you would honestly wonder what planet they live on, and be totally blown away by how different their “reality” is from yours.
You’d also never, in a million years, be quick to judge again.
Just sayin’
The Universe
(Mike Dooley www.tut.com)
PFI interest rates by bailed-out banks unjustified
NEWS FROM THE CENTRE FOR INTERNATIONAL PUBLIC HEALTH POLICY
PFI interest rates by bailed-out banks unjustified
http://bit.ly/Qtbe5
http://www.health.ed.ac.uk/CIPHP/
The UK government is allowing banks to restore their profits by charging unjustifiably high interest rates for health service private finance initiative (PFI) projects, a study claims.
An opportunity to negotiate better interest rates is being missed, researchers suggest, now that two banks providing investment for new hospitals are partly owned by the government.
As a result, say researchers at the University of Edinburgh, the quality and financial performance of NHS services are being impaired.
The study analysed the 149 major PFI hospital projects that have been signed by the NHS so far. The researchers found that two banks in which the government is the major shareholder – Royal Bank of Scotland and Lloyds – have provided senior debt (the low interest portion of the borrowing) to 38 projects and have equity in 16.
The researchers say that these projects have raised £12.27 billion under PFI – but that over the next 30 to 60 years, the public sector will pay a total of £41 billion for the cost of capital alone.
Prof Allyson Pollock, of the University of Edinburgh’s Centre for International Public Health Policy, said: “Instead of using the opportunity of the taxpayer bail-out to reopen the contracts and negotiate better rates in favour of the public sector, the UK government is allowing the banks to restore their balance sheet by charging relatively high rates of interest for PFI schemes.
“The increased costs of servicing the debt are met from annual budgets of the NHS, and result in reductions in the money available for services.”
Prof Pollock said that the policy of using private finance is used to disguise public expenditure liabilities, since it takes capital investment off the government’s books. International accounting rules that would have required government to put PFI back on the balance sheet are being ignored.
She added: “The policy is expensive; compared with conventional government borrowing and procurement, PFI is associated with high costs of borrowing which include high rates of returns to the investors.
“There is a risk that reductions in public expenditure could provide a new political impetus for using PFI regardless of whether the policy is socially and economically beneficial and this will continue to be at the expense of major reductions in public services and public expenditure cuts.”
For further information, please call
Prof Allyson Pollock, Centre for International Public Health Policy
+44 (0)131 651 3964; +44 (0)7976 978304
allyson.pollock@ed.ac.uk
Why Can’t Americans Get Health Care Right?
Good piece from Harvard Business Review by Jim Heskett. I particularly enjoyed the reasoned and balanced opinions that follow.
Read it here: hbswk.hbs.edu/item/6245.html
Oral Cancer Rates Up – but is the real truth hard to swallow?
There have been a lot of mentions in the media over the past 10 days that the rates of Oral Cancer have risen in individuals in their 40s.
When I was a student & during my hospital career we were told that Oral & Lip Cancers were related to the “5Ss”:
- Smoking,
- Spirits,
- Sepsis,
- Sunshine
- Syphilis.
Of these without doubt the greatest cause was and remains smoking; spirits were usually blamed but heavy drinkers frequently smoked heavily and there was a synergistic effect of the two. Sepsis was implicated because frequently victims were in poor condition already and heavy smokers’ mouths were never the best with widespread gum disease. Sunshine without doubt led to an increase in tumours of lips & facial skin. Syphilis well that shows my vintage; however we seem to retain some of our puritan attitude to talking about sex.
The recent news has picked, as ever, on the easy target ‘Alcohol To Blame For Rise In Oral Cancers’ said the Sky News headline, ‘A sober look at the rise in mouth cancer’ in The Times blames binge-drinking, a phrase that has only been in use for a few years far too soon for the effects to be measured properly. It is impossible to properly understand an epidemic until it is over.
As ever the anti-booze bandwagon has used this information to threaten doom, but whilst most reports mention there could be involvement of the human papilloma virus it gets very little publicity. As long ago as Feb 2004 BBC News reported “Oral Sex Linked To Mouth Cancer”. This is the same virus implicated in cervical cancer and causes genital warts, a vaccine is available and should be given to both girls and boys before they become sexually active. This much we can do easily and far easier than persuading sexually active and experimental young people into changing habits. I realise that the nay-sayers will tell you that it leads to promiscuity as it removes the fear of infection but that is really an unrealistic argument.
A recent study conducted by Dr. Maura Gillison at the Johns Hopkins Oncology Center furthered the premise that HPV is linked with certain types of oral cancer. In 25% of 253 patients diagnosed with head and neck cancers, the tissue taken from tumors was HPV positive and HPV 16 was present in 90% of these positive HPV tissues. This information helps to confirm that there is a strong link between HPV 16 and oral cancer. 25% of those diagnosed with oral cancer are non-smokers while the other 75% of those diagnosed have used tobacco in some form during their lifetimes. The research into the relationship of HPV and oral malignancies may give us clues as to the origin of cancer in those 25% of diagnosed individuals who did not smoke. Further research is being conducted into the relationship of HPV with oral cancers.
The habits that dare not speak their name?